The proportion of men choosing active surveillance (AS) over surgery or radiotherapy for prostate cancer has increased approximately threefold in the USA since 2010, but researchers from Vanderbilt University Medical Center and University Hospitals (UH) Cleveland Medical Center believe further improvements could still be made.
The findings are based on an analysis of data from the Surveillance, Epidemiology and End Results Prostate with Watchful Waiting database and included 74,103 men diagnosed with low-risk prostate cancer, as defined by the National Comprehensive Cancer Network, between 2010 and 2018 and 31,699 men with favorable intermediate-risk disease.
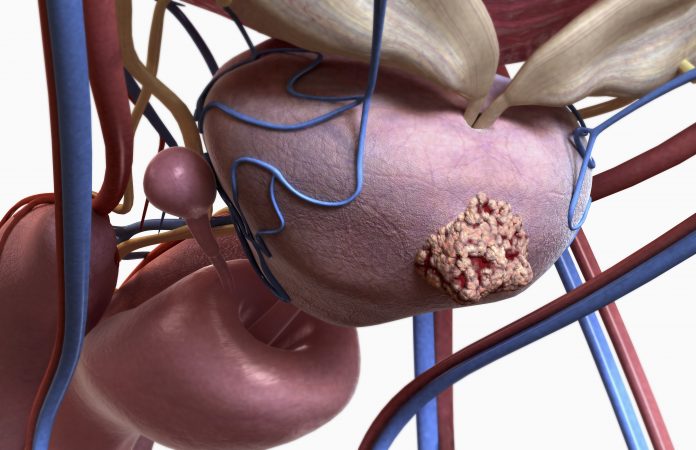
Men with low-risk prostate cancer are generally eligible for AS, senior author Jonathan Shoag, MD, associate professor of Urology at UH Seidman Cancer Center in Cleveland, UH Urology Institute, and Case Western Reserve University, and lead author Bashir Al Hussein Al Awamlh, MD, from Vanderbilt, told Inside Precision Medicine.
However, they added that some factors, such as a large lesion with a high Prostate Imaging Reporting and Data System (PI-RADS-5) score on magnetic resonance imaging (MRI), would make them “nervous” about taking that approach as these features can lead to a worse outcome on surveillance.
For favorable intermediate-risk cancers, there are different criteria for AS depending on the guideline panels, institutions, and protocols.
“Some would say all favorable intermediate-risk patients are eligible for surveillance. I think many of us try to get a sense of the volume and aggressiveness of cancer using MRI, the percentage of cores that are positive, and the percentage of Gleason pattern 4 on biopsy, which in my mind is a major determinant,” said Shoag.
He added that according to the European Association of Urology guidelines, individuals with cribriform and intraductal histology should be excluded from AS and highlighted that there is a difference between low risk and low (Gleason) grade–not all low-grade cancers are low risk.
The researchers report in JAMA Internal Medicine that the proportion of men with low-risk disease who opted for AS or watchful waiting (WW), which differs from AS in that cancer is not monitored for progression but observed until it becomes symptomatic, increased significantly from 16.4% in 2010 to 59.9% in 2018.
For those with favorable intermediate-risk cancers, the AS rate increased significantly from 7.8% to 21.8%.
Shaog and Al Hussein Al Awamlh said that these increases are a result of “a real effort by some of the greats in our field, like Laurence Klotz and Gerald Chodak, who recognized that many of the cancers we were treating probably could be observed.
“This led to large academic series of active surveillance that showed it was safe, particularly for low-risk men, and most recently randomized trial data which largely have confirmed that. All of this has occurred concurrent with changes in guidelines on how to manage these patients.”
Nonetheless, the investigators note that AS rates in the USA are still lower than those in other countries such as Australia, where the rates were 67% in 2016, and Sweden, at 74% in 2014.
The reasons for this are “probably multifactorial,” noted Shaog and Al Hussein Al Awamlh. “To a certain extent the US is just a much bigger and [more] diverse population–both in terms of patients and physicians, so uniformity in practice here for many things is likely more difficult to achieve.”
The researchers also observed some disparities in the uptake of active surveillance among certain subgroups of the US patients.
“We found particularly Asian/Pacific islander, Hispanic men, and men living in rural areas were less like to undergo surveillance, not necessarily all minority men,” said Shoag.
“Whether this reflects cultural preferences by the patient, or a lack of education for their providers is uncertain. I can tell you I have a fair number of patients who are farmers. Some of them just want their cancer out and done with based on their lifestyle and preferences and don’t want to undergo surveillance because of the steps involved.”
Multivariate analyses among these groups showed that Asian/Pacific islander men with low-risk cancer were 24% less likely that Non-Hispanic White men to opt for AS or WW while Hispanic men were 31% less likely. The corresponding odds were 36% and 25% lower among men with favorable intermediate-risk disease.
Men with low-risk disease living in rural counties were 12% less likely than those in urban areas to undergo AS or WW, but there was no significant difference by county among the men with favorable intermediate-risk cancers.
Other differences observed in the multivariate analyses included a decreasing trend for AS or WW with an increasing number of positive biopsy cores (≥2 vs 1), but an increasing likelihood with a greater number of cores examined (≥12 vs ≤11). Individuals with a lower median household income (≤$74,999) were 24& to 30% less likely to choose AS or WW than those with a higher income.
Shaog and Al Hussein Al Awamlh said they believe AS “gives us a chance to watch a cancer and see how it behaves over time with the plan that we will intervene if needed.”
They added: “Some would advocate the use of genomic biomarkers to determine surveillance eligibility. There may be a role for this in some cancers, but for low-risk cancers which we know are safe to watch in the absence of genomics, I don’t think these are beneficial—all they do in this context is push us towards treatment. The goal should be to minimize the morbidity of treatment in as many men as is safe to do so.”
And although the study only includes data up to 2018, the authors said they “would hope the rate [of AS uptake] would continue to increase.”






![AI Algorithm Could Reduce Breast Cancer Mammogram False Positive Rate The primary goal of the Paradigm Registry is to accelerate tumor profiling based on disease biology. [iStock/LilliDay]](https://www.insideprecisionmedicine.com/wp-content/uploads/2019/01/307-218x150.jpeg)






