Abstract
To compare the effectiveness of self- retained cryopreserved AM as an adjuvant therapy for infectious corneal ulcers. Retrospective, case–control study of 24 eyes of 24 consecutive patients with central and paracentral corneal infectious ulcers and initial visual acuity worse than 20/200. Among them, 11 eyes of 11 patients received additional placement of self-retained cryopreserved AM. Epithelialization and Best Corrected Snellen Visual Acuity (BCSVA) were compared between the two groups. At baseline, both groups had comparable age, gender, visual acuity (VA), size and location of corneal ulcer. Patients receiving additional placement of cryopreserved AM had significantly faster epithelialization within 3.56 ± 1.78 weeks vs 5.87 ± 2.20 weeks (p = 0.01) and achieved complete epithelialization in significantly more patients (72.7% vs 23.1% p = 0.04) despite overall larger baseline defect size (32.7 ± 19.5 mm2 vs 21.5 ± 10.7 mm2, p = 0.11). Consequently, the AM group had clinically significant BCSVA (> 3 lines) (81.8% vs 38.4%, p = 0.047) and total VA improvement (log MAR 0.7 ± 0.6 vs 1.6 ± 0.9, p = 0.016) compared to the control group at the time of complete epithelialization. In-office sutureless AM may be an effective adjuvant therapy in treating sight-threatening infectious corneal ulcers by promoting faster corneal epithelialization and overall better recovery of the VA.
Similar content being viewed by others
Introduction
The corneal epithelium acts as the first line of immunological defense and plays an important role in serving the optical interphase with the tear film. When this protective barrier is subjected to endogenous (e.g., severe inflammation) or exogenous (e.g., mechanical) insults, this may cause punctate erosion, which eventually evolves into a corneal epithelial defect1. If not treated appropriately and promptly, the persistent corneal defect can progress to severe vision-threatening complications such as infectious corneal ulcer, perforation, and endophthalmitis.
Early diagnosis and treatment of the underlying cause of the corneal ulcer are essential in restoring the ocular surface health. For infectious cases, proper topical or systemic anti-microbial therapies are required along with discontinuation of other inappropriate medications, especially topical medications with preservatives that may cause medicamentosa, i.e., ocular toxicity. To further support epithelial wound healing, adjunctive measures are implemented such as tarsorrhaphy, bandage contact lens, and amniotic membrane (AM) transplantation. Of these choices, AM not only delivers steroid-sparing anti-inflammatory, anti-scarring, and pro-regenerative properties2,3 but also provides a mechanical protective barrier effect. Suture of cryopreserved AM in the operating room4,5,6 or placement of self-retained cryopreserved AM in-office7,8,9,10 has successfully treated corneal ulcers of various etiologies. However, comparative analysis between self-retained AM and a control group has not been performed. Herein, we report the first case-controlled study to compare treatment for central and paracentral corneal infectious ulcers with the standard of care alone with and without additional placement of self-retained cryopreserved AM.
Materials and methods
This study was approved by the SUNY Upstate State Medical University Institutional Review Boards [1593072-1]. Written informed consent was obtained in advance from all patients in accordance with the principles expressed in the Declaration of Helsinki for human subjects. A retrospective chart review was performed on consecutive patients with severe central or paracentral corneal infectious ulcers of the size of > 4mm2 and vision worse than 20/200 and were treated between 2016 and 2020 at SUNY Upstate Medical University. Any patient with lagophthalmos, eyelid abnormality, Bell's palsy, severe ectropion, descemetocele found to be high risk for perforation, or perforated corneal ulcer were excluded from this study. Prior to 2018, amniotic membrane utilization was not adopted by SUNY Upstate. Once self retained amniotic membrane was adopted at Upstate after 2018, patients were given the choice of amniotic membrane as an adjuvant therapy.
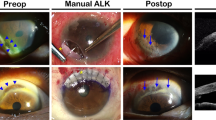
All patients received the standard of care including corneal scraping and microbiological culture before receiving topical broad-spectrum antimicrobial antibiotics (Vancomycin 25 mg/ml and Tobramycin 15 mg/ml). Once culture was confirmed, target antimicrobial therapy was given. For bacterial keratitis, patients received oral fluoroquinolone 500 mg twice daily for 10 days. For fungal keratitis, patients received topical fortified voriconazole or amphotericin B ophthalmic drops and a 10-day course of oral Voriconazole. For viral keratitis, patients received topical Ganciclovir and 14-days of oral valacyclovir 500 mg 3 times daily. Patients in the AM group received additional placement of cryopreserved AM, i.e. PROKERA Slim (Bio-Tissue, Inc, Miami, FL), in the office under topical anesthesia with 0.5% proparacaine hydrochloride eye drops. Briefly, cryopreserved AM was rinsed with a sterile balanced salt solution. Then, with the patient in a seated position, cryopreserved AM was gently inserted into superior fornix while the patient was looking down and AM centered covering the ulcerated defect after the patient resumed the orthophoric gaze. No additional fixation was used to secure the cryopreserved AM such as lateral tarsorrhaphy or external tape. Cryopreserved AM was left for at least 5 days and the membrane ring was gently removed using small tooth-forceps. Patients were followed daily for the first week, and then at least weekly thereafter.
The primary outcome measure was the proportion of patients that achieved complete corneal epithelialization, which was also determined by the absence of any fluorescein staining. Improvement of visual acuity (more than 1 line improvement or at least 3-line improvement) was also evaluated at 1 month as well at the time of complete epithelialization.
The statistical analyses were carried out using SPSS Software version 20 (IBM; Armonk, NY). Continuous data are reported as mean ± standard deviation and categorical data are reported as percentage. Data between treatment groups were compared using Fisher exact test and t-test for categorical data and continuous data, respectively. A p value < 0.05 was considered statistically significant.
Results
A total of 24 eyes of 24 patients were included and consisted of 13 eyes of 13 patients receiving the standard of care alone and 11 eyes of 11 patients receiving additional placement of self-retained cryopreserved AM. The baseline demographic data and preoperative characteristics of all patients are summarized in Tables 1 and 2. Aside from an average younger age in the AM group (45.5 ± 13.9 vs 61.2 ± 21.6, p > 0.05), both groups had similar proportion of males vs. females (p = 0.21) and baseline vision (p = 0.63). At the baseline, the AM group had more centrally located ulcer 8 out of 11 eyes (72%) than control group 7 out of 13 (53%), however it was not statistically significant (p = 0.42). Additionally, the baseline corneal ulcer area of the AM group was overall larger than that of the control group although not statistically significant (32.7 ± 19.5 mm vs 21.5 ± 10.7 mm, p = 0.11).
For the patients receiving additional self-retained cryopreserved AM, bacterial keratitis was noted in 9 eyes, fungal keratitis in 1 eye, and herpes simplex virus keratitis in 1 eye. For patients receiving the standard of care only, cultured proven bacterial keratitis was noted in 8 eyes, fungal keratitis was confirmed in 1 eye while presumed bacterial keratitis was found in the remaining 4 eyes. The proportion of infectious cause was not statistically significant between the two groups (p = 0.65).
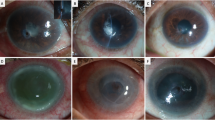
At one-month follow-up, 72.7% of the eyes in the AM group had complete epithelialization compared to 23.1% in the control group (p = 0.04). By 2 months, 100% of eyes were healed in AM group compared to 84.6% in the control group (p = 0.46). By 3 months, all ulcers were healed in both groups. Patients treated with AM showed faster epithelialization within an average 3.6 ± 1.8 weeks compared to 5.9 ± 2.2 weeks in the control group (p = 0.01).
At 1 month, the BCSVA was improved at least 1 line in 10 of the 11 eyes (90.9%) in the AM group compared to 6 of the 13 eyes (46.1%) in the control group receiving the standard of care (p = 0.03). Nine out of 11 eyes (81.8%) in the AM group achieved 3 lines or better in their BCSVA compared to 5 of the 13 eyes (38.4%) in the control group (p = 0.047). At the time of complete epithelialization, 11 of 11 (100%) eyes in the AM group showed at least 1-line improvement compared to 6 of the 13 eyes (46.1%) in the control group (p = 0.006). Nine of 11 eyes (81.8%) achieved 3 lines or better in the AM group compared to 5 out of 13 eyes (38.4%) in the control treatment group (p = 0.047). Vision significantly improved from pretreatment logMAR 2.3 ± 0.3 to final VA of 0.7 ± 0.6 (p < 0.00001) in the AM group, while VA improved from pretreatment logMAR 2.3 ± 0.3 to final VA of 1.6 ± 0.9 (p = 0.008) in the control group. The AM group showed more total VA improvement compared to control (log MAR 0.7 ± 0.6 vs 1.6 ± 0.9, p = 0.016). Neither group had worsened visual acuity and all cases of hypopyon resolved. Therefore, eyes receiving additional placement of self-retained cryopreserved AM showed faster complete epithelialization and clinically significant BCSVA improvement (1 line, > 3 lines, and total) compared to the control group. No complications were observed with the use of AM, aside from foreign body sensation.
Discussion
The use of sutureless self-retained cryopreserved AM allows early intervention as it can be performed in the office not only to facilitate the treatment but also to reduce the overall cost. Previously, a number of reports have shown the effectiveness of single15,16,18,19,20,21,22,26,27,29,32 or multiple15,16,17,18,20,21,22,23,24,25,26,27,28,30,31,33 layers of sutured AM for infectious5,6,15,16,17,18,19,20,21,22,23,25,27,28,33 or non-infectious15,17,18,21,22,23,24,25,26,28,29,30,31,32 corneal ulcers and several reports have similarly shown the effectiveness of sutureless AM for infectious7,8,9,10 and non-infectious7,12,13,14 corneal ulcers. The three retrospective case series7,8,9,10 that evaluated self-retained AM for infectious corneal ulcers showed healing in 66–100% of cases in as little as 4 days along with reduced ocular surface inflammation and improved VA during 3–51 months of follow-up. Herein, we present the first retrospective control study to support that additional placement of sutureless self-retained cryopreserved AM in conjunction with the standard of care is effective in promoting significantly faster epithelialization and better visual acuity than that by the standard of care alone.
Taken together, the aforementioned cumulative clinical evidence is in alignment with the unique steroid-sparing anti-inflammatory, anti-scarring, and pro-regenerative properties of AM10,11. Although AM is known to contain multiple extracellular matrix components and growth factors that could contribute to these properties, research efforts supported by the National Institutes of Health over the last decade have led to the discovery of heavy chain 1 [derived from inter- α-trypsin inhibitor]–HA/pentraxin 3 (HC–HA/ PTX3) as the major active tissue component that is responsible for AM’s “multiple” therapeutic actions that extend to a number of cell types (reviewed in2). In brief, HC-HA/PTX3′s anti-inflammatory action works through modulating activated but not resting neutrophils, macrophages, and lymphocytes extending from innate to adaptive immune responses. This is in contrast to steroids which is known to manifest dose-dependent adverse event leading to immunocompromised state, inhibition of epithelialization, and risk of corneal melting.
This steroid-sparing anti-inflammatory effect is particular palatable in managing corneal ulcers which have an infection as the underlying cause, and may explain why placement of self-retained cryopreserved AM is beneficial in promoting corneal epithelial healing despite the baseline corneal ulcer area was relatively larger. In addition, HC-HA/PTX3′s anti-scarring action, demonstrated in human corneal fibroblasts by downregulating the TGF-β1 promoter activity34 and its anti-angiogenic action by inhibition of endothelial tube formation35 may help explain why the resultant visual acuity is better in the AM group despite the baseline corneal ulcers were more centrally located.
Finally, corneal ulcer disrupts the integrity of the ocular surface, which can result in further damage from the mechanical friction. The cryopreserved AM may serve as a safe mechanical barrier, preventing further fricational trauma to the ocular surface. Furthermore, various studies have reported AM to retain an antimicrobial property36,37,38,39. If confirmed, this may also suggest why the epithelialization occurred much faster in the AM group. Yet it remains unknown whether AM contains antimicrobial properties or simply enhances the delivery of fortified medications to the ocular surface40,41. Further prospective and randomized control studies could help to confirm the efficacy of self-retained cryopreserved AM and as an adjunctive treatment for infectious corneal ulcers.
References
Bukowiecki, A., Hos, D., Cursiefen, C. & Eming, S. A. Wound-healing studies in cornea and skin: parallels, differences and opportunities. Int. J. Mol. Sci. 18, 1257 (2017).
Tseng, S. C. HC-HA/PTX3 purified from amniotic membrane as novel regenerative matrix: insight into relationship between inflammation and regeneration. Invest Ophthalmol Vis Sci. 57, ORSFh1-8 (2016).
Tseng, S. C. et al. How does amniotic membrane work?. Ocular Surf. 2, 177–187 (2004).
Liu, J., Li, L. & Li, X. Effectiveness of cryopreserved amniotic membrane transplantation in corneal ulceration: a meta-analysis. Cornea 38, 454–462 (2019).
Schuerch, K., Baeriswyl, A., Frueh, B. E. & Tappeiner, C. Efficacy of amniotic membrane transplantation for the treatment of corneal ulcers. Cornea 39, 479–483 (2020).
Lee, S. H. & Tseng, S. C. Amniotic membrane transplantation for persistent epithelial defects with ulceration. Am. J. Ophthalmol. 123, 303–312 (1997).
Suri, K. et al. Sutureless amniotic membrane ProKera for ocular surface disorders: short-term results. Eye Contact lens. 39, 341–347 (2013).
Cheng, A. M. & Tseng, S. C. Self-retained amniotic membrane combined with antiviral therapy for herpetic epithelial keratitis. Cornea 36, 1383–1386 (2017).
Sheha, H., Liang, L., Li, J. & Tseng, S. C. Sutureless amniotic membrane transplantation for severe bacterial keratitis. Cornea 28, 1118–1123 (2009).
Sheha, H., Tighe, S., Cheng, A. M. & Tseng, S. C. A stepping stone in treating dendritic keratitis. Am. J. Ophthalmol. Case Rep. 7, 55–58 (2017).
Patel, H. et al. The New Zealand national eye bank: survival and visual outcome 1 year after penetrating keratoplasty. Cornea 30, 760–764 (2011).
McCourt, E. A., Wei, L. A., Richards, S., Taravella, M. J. & Enzenauer, R. W. A novel use of amniotic membrane for the treatment of bilateral corneal ulcers due to severe Vitamin A deficiency in an autistic child. Invest. Ophthalmol. Vis. Sci. 53, 1870–1870 (2012).
Kassm, T. M. & Ursea, R. The value of amniotic membrane patch in the treatment of corneal thinning as assessed by anterior segment optical coherence tomography. Invest Ophthalmol. Vis. Sci. 55, 2466–2466 (2014).
Pachigolla, G. et al. Evaluation of the role of ProKera in the management of ocular surface and orbital disorders. Eye Contact Lens. 35, 172–175 (2009).
Chen, H. J., Pires, R. T. & Tseng, S. C. Amniotic membrane transplantation for severe neurotrophic corneal ulcers. Br. J. Ophthalmol. 84, 826–833 (2000).
Ma, D. H., Wang, S. F., Su, W. Y. & Tsai, R. J. Amniotic membrane graft for the management of scleral melting and corneal perforation in recalcitrant infectious scleral and corneoscleral ulcers. Cornea 21, 275–283 (2002).
Solomon, A. et al. Amniotic membrane grafts for nontraumatic corneal perforations, descemetoceles, and deep ulcers. Ophthalmology 109, 694–703 (2002).
Hick, S. et al. Amniotic membrane transplantation and fibrin glue in the management of corneal ulcers and perforations: a review of 33 cases. Cornea 24, 369–377 (2005).
Chen, H. C. et al. Amniotic membrane transplantation for persistent corneal ulcers and perforations in acute fungal keratitis. Cornea 25, 564–572 (2006).
Heiligenhaus, A. et al. Management of acute ulcerative and necrotising herpes simplex and zoster keratitis with amniotic membrane transplantation. Br. J. Ophthalmol. 87, 1215–1219 (2003).
Yang, J. et al. Surgical treatment of 32 cases of long-term atopic keratoconjunctivitis using the amniotic membrane. Eye 27, 1254 (2013).
Park, J. H. et al. Clinical efficacy of amniotic membrane transplantation in the treatment of various ocular surface diseases. Cont. Lens Anterior Eye. 31, 73–80 (2008).
Khokhar, S. Amniotic membrane transplantation in refractory neurotrophic corneal ulcers: a randomized, controlled clinical trial. Cornea 24, 654–660 (2005).
Hanada, K. et al. Multilayered amniotic membrane transplantation for severe ulceration of the cornea and sclera. Am. J. Ophthalmol. 131, 324–331 (2001).
Kruse, F. E., Rohrschneider, K. & Volcker, H. E. Multilayer amniotic membrane transplantation for reconstruction of deep corneal ulcers. Ophthalmology 106, 1505–1511 (1999).
Meller, D. et al. Amniotic membrane transplantation for acute chemical or thermal burns. Ophthalmology 107, 980–990 (2000).
Kim, J. S. et al. Amniotic membrane transplantation in infectious corneal ulcers. Cornea 20, 720–726 (2001).
Prabhasawat, P., Tesavibul, N. & Komolsuradej, W. Single and multilayer amniotic membrane transplantation for persistent corneal epithelial defect with and without stromal thinning and perforation. Br. J. Ophthalmol. 85, 1455–1463 (2001).
Tu, P. & Hou, Y. C. Bilateral corneal melting associated with topical diclofenac 0.1% after cataract surgery in a patient with Sjögren’s syndrome. Taiwan J. Ophthalmol. 9, 202–205 (2019).
Rock, T., Bartz-Schmidt, K. & Rock, D. Management of a neurotrophic deep corneal ulcer with amniotic membrane transplantation in a patient with functional monocular vision. A case report. Medicine 96, e8997 (2017).
Nicula, C. & Szabo, I. Complicated corneal ulcer. Case report. Rom. J. Ophthalmol. 60, 260–263 (2016).
Burcu, A., Dogan, E., Yalniz-Akkaya, Z. & Ornek, F. Early amniotic membrane transplantation for toxic keratopathy secondary to topical proparacaine abuse: a report of seven cases. CutanOcul. Toxicol. 32, 241–247 (2013).
Hoffmann, S., Szentmáry, N. & Seitz, B. Amniotic membrane transplantation for the treatment of infectious ulcerative keratitis before elective penetrating keratoplasty. Cornea 32, 1321–1325 (2013).
He, H. et al. Biochemical characterization and function of complexes formed by hyaluronan and the heavy chains of inter-a-inhibitor (HCHA) purified from extracts of human amniotic membrane. J.Biol. Chem. 284, 20136–20146 (2009).
Shay, E., He, H., Sakurai, S. & Tseng, S. C. Inhibition of angiogenesis by HC·HA, a complex of hyaluronan and the heavy chain of inter-α-inhibitor, purified from human amniotic membrane. Invest. Ophthalmol. Vis. Sci. 52, 2669–2678 (2011).
Kjaergaard, N. et al. Antibacterial properties of human amnion and chorion in vitro. Eur. J. Obstet Gynecol. Reprod. Biol. 94, 224–229 (2001).
Palanker, N. D. et al. Antimicrobial efficacy assessment of human derived composite amnion-chorion membrane. Sci. Rep. 9, 15600 (2019).
Mao, Y. et al. Antimicrobial peptides secreted from human cryopreserved viable amniotic membrane contribute to its antibacterial activity. Sci. Rep. 7, 13722 (2017).
Zare-Bidaki, M., Sadrinia, S., Erfani, S., Afkar, E. & Ghanbarzade, N. Antimicrobial properties of amniotic and chorionic membranes: a comparative study of two human fetal sacs. J. Reprod. Infertil. 18, 218–224 (2017).
Mencucci, R., Paladini, I., Menchini, U., Gicquel, J. J. & Dei, R. Inhibition of viral replication in vitro by antiviral-treated amniotic membrane. Possible use of amniotic membrane as drug-delivering tool. Br. J. Ophthalmol. 95, 28–31 (2011).
Mencucci, R., Menchini, U. & Dei, R. Antimicrobial activity of antibiotic-treated amniotic membrane: an in vitro study. Cornea 25, 428–431 (2006).
Funding
No Funding was received for this research study. No authors have any financial interest in this study.
Author information
Authors and Affiliations
Contributions
H.Y. and S.A. designed the study and carry out the treatments. H.Y., A.C, S.T,S.A wrote the introduction, design and discussion. "P.K. and J.N. collected the clinical data prepared table 1 and 2. H.Y. and S.D. help with the statistical analysis. H.Y., S.A., R.S. treated and followed up the patient's results in each visits. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yin, H.Y., Cheng, A.M.S., Tighe, S. et al. Self-retained cryopreserved amniotic membrane for treating severe corneal ulcers: a comparative, retrospective control study. Sci Rep 10, 17008 (2020). https://doi.org/10.1038/s41598-020-73672-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-73672-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.