Abstract
Background
The coronavirus SARS-CoV-2 is highly contagious. Hydroxychloroquine (HCQ) has in vitro activity against SARS-CoV-2. The FDA authorized emergency use of HCQ against COVID-19. HCQ may have dose-related cardiotoxicity. This clinical trial received ethical approval on May 15, 2020, operationalized in June to evaluate a low prophylaxis dose of HCQ (200mg BID) in household contacts of COVID-19-positive patients without physical contact between investigators and participants. It represents the first report of the FDA approved 6-lead EKGs with a smartphone KardiaMobile® 6L application.
Methods
To reach a sample size of 170, household members were contacted by telephone, emailed consent forms with electronic signature capability, and randomized 2:1 to HCQ or observation for 10 days with follow-up of 14 days. Home saliva PCR tests recorded COVID status on days 1 and 14. Symptoms and 6-lead EKGs were obtained daily.
Results
Fifty-one participants were randomized with 42 evaluable at day 14. Remote monitoring of 407 EKGs revealed no QTc prolongation or other ECG changes in either group. At time of consent, no participants were symptomatic or COVID+. On days 1 and 14, COVID tests were positive in 4 and 2 in the HCQ group and 4 and 0 in the observation group. No tests converted to positive. There were no deaths or hospitalizations.
Conclusions
A clinical trial without personal contact, rapidly initiated and operationalized to exclude cardiac toxicity using daily remote 6-lead EKG monitoring, is feasible. Of 407 EKGs from 42 participants, there was no evidence of cardiac toxicity.
Clinical trial registration
Clinicaltrials.gov: NCT04652648 registration date: December 3, 2020
Similar content being viewed by others
1 Introduction
The world remains consumed by the COVID-19 pandemic caused by coronavirus SARS-CoV-2 [1]. The virus produces significant morbidity and mortality and is highly contagious [2]. The first patients with COVID-19 infections were admitted to the hospitals of the Main Line Health System in March 2020. The admission rate quickly rose to over 30 cases/day by the end of the month. At that time, the virus was known to spread mainly by respiratory droplets [3] with a median incubation period of approximately 5 days [4]. Infection rates in contacts of active COVID-19 patients were estimated as high as 50–75%, but many patients remained asymptomatic [5], complicating assessment.
Vaccines are the ultimate solution to COVID prevention. Providing vaccines globally has been a challenge. Wearing appropriate masks and physical distancing remain an effective means of preventing SARS-CoV-2 transmission. Chloroquine derivatives have been proposed as preventative agents against the virus, expanding their well-known prophylactic role against malaria parasites [6]. There are reports of the in vitro activity of several drugs against SARS-CoV-19, which include hydroxychloroquine (HCQ) [7,8,9,10,11,12]. A proposed mechanism of action was elevation of the pH of acidic intracellular organelles inhibiting membrane fusion and viral entry [9].
Fortunately HCQ was readily available thus allowing a study to test efficacy of oral HCQ prophylaxis of household contacts of COVID-19 positive patients. A US Food and Drug Administration (FDA) emergency use authorization of HCQ to treat COVID-19 was also in effect allowing many patients to be treated outside formal study protocols, without standardized dosing and without systematic data collection to address safety and efficacy. At the time, N-95 masks and hospital beds were in critically short supply, and many potential enrollees were quarantined at home and/or reluctant to travel to a hospital or outpatient center for screening, enrollment, and required studies. Thus this study was conducted entirely without physical contact to protect spread in general but specifically toward health care providers.
Studies conducted without personal contact have become more common with the continued development of connected medical devices [13,14,15]. These studies were always planned well in advance of trial initiation. In this trial, the mandate to avoid personal contact posed unique challenges for both investigators and potential participants, with limited time for implementation and recruitment. Obtaining informed consent remotely was particularly challenging during the COVID-19 pandemic. This was partly related to the large volume of constantly changing publicly available information on COVID-19 drug treatment and prophylaxis. SARS-CoV-2 self-testing at home also relied on the availability of an assay newly approved by the Food and Drug Administration. Reliable shipping services to deliver study drug and to deliver and return coronavirus test kits within a specified timeline were also critical.
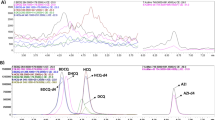
Cardiac involvement by SARS-CoV-2 was becoming evident [16], and HCQ was known to prolong QTc and trigger arrhythmias [17]. This was more often seen at higher doses of HCQ, frequently with concomitant azithromycin use, and in COVID-19-positive, hospitalized patients [18]. Thus, obtaining high-quality EKGs for participants on-treatment and for those in the control group in the home setting was critical. EKG monitoring via smartphone or smartwatch applications [19] has become commonplace, and large-scale studies have been conducted to validate the performance of these devices [20]. However, not all devices are approved for assessment of clinical trial endpoints including QTc measurements. Shortly before the start of this trial, the FDA granted emergency use authorization for the use of the KardiaMobile® 6L device [21] for remote QTc assessments (Fig. 1). Enrollees in this trial were likely to be technology-naive regarding smartphone-facilitated EKG monitoring, necessitating the need for remote training [22,23,24]. Maintaining data privacy while using remote monitoring was a concern [25]. The FDA has provided guidance on the use of medical devices during the COVID-19 public health emergency [26], stressing the safety of participants and confidentiality of data.
2 Methods
Study design
The Institutional Review Board of the Main Line Health Hospitals, Wynnewood, Pennsylvania, approved an open-label trial randomizing participants 2:1 to HCQ 200 mg orally twice a day for 10 days or to observation; both groups were followed for a total of 14 days. SARS-CoV-2 PCR testing was conducted at enrollment and then 14 days later. Participants were questioned regarding possible COVID-19 symptoms at five timepoints during the 14-day study. The primary endpoints were the development of COVID-19 symptoms with a positive coronavirus PCR test by day 14, the development of a positive coronavirus PCR test without symptoms by day 14, hospital admission by day 14, death by day 14, and EKG evidence of cardiotoxicity in both the HCQ group and the observation group.
Inclusion and exclusion criteria
Hospitalized patients with positive COVID-19 nasal PCR tests were identified by infectious diseases physicians. Permission was obtained to contact their household members.
Specific inclusion criteria
Exposure to a COVID-19-infected individual in the same household within 5 days of diagnosis; age >18 years; ability to give informed consent to participate in a clinical study; ability to swallow oral medications; and access to a smartphone.
Exclusion criteria
Allergy or intolerance to HCQ (Plaquenil®); weight less than 85 lb; eye disease affecting the retina; severe kidney or liver disease; G6PD-deficiency; porphyria; long QTc EKG abnormality or family history of long QTc abnormality and other major EKG abnormalities; taking medications that can affect the QT interval including flecainide, amiodarone, digoxin, procainamide, propafenone, sotalol, quinidine, dofetilide, levofloxacin, ciprofloxacin, azithromycin, erythromycin, amitriptyline, doxepin, desipramine, imipramine, fluoxetine, sertraline, venlafaxine, quetiapine, haloperidol, droperidol, thioridazine, ziprasidone, furosemide, sumatriptan or zolmitriptan, cisapride, arsenic, dolasetron, or methadone; current pregnancy; current hospitalization; symptomatic with fever or cough; and lack of access to a smartphone.
Informed consent
Consent from individuals meeting enrollment criteria was obtained by telephone and documented by electronic signing of IRB-approved consent and HIPAA authorization forms. A baseline health and symptom questionnaire was administered by telephone by the study coordinator upon enrollment. Participants were told to maintain self-quarantine as per public health department orders for contacts of COVID-19 cases.
Home coronavirus testing
A saliva RNA PCR test for COVID-19 recently approved by the FDA was chosen as less uncomfortable and easier to perform as a home technique compared with nasal swab-based tests. After informed consent was obtained, home SARS-CoV-2 saliva rapid tests (Accurate Diagnostics Lab, South Plainfield, NJ, USA) were shipped to enrollees with instructions for sample acquisition and shipping using prepaid envelopes on day 1 and day 14.
Home EKG monitoring
KardiaMobile® EKG monitoring software (AliveCor, Mountain View, CA) (Fig. 1) was downloaded by study enrollees to their smartphones. A 6-lead hardware monitoring pad for attachment to the phone was shipped to each enrollee’s household. Instructions were provided by the clinical study coordinator to submit an EKG tracing 1 h before taking the first dose of study drug and then approximately 2 h after that dose and then daily. For individuals in the observation group, a single EKG tracing was required daily.
The KardiaMobile® device is capable of obtaining either a single-lead tracing or a six-lead tracing. The tracing is recorded for the time period defined by the settings on the Kardia smartphone application. The tracing is automatically saved, downloaded in pdf format, and emailed for interpretation to the cardiologist study investigator. Quality of the EKGs depended upon the enrollee’s ability to complete the required steps, which resulted in both good quality and poor quality EKGs (Figs. 2, 3, 4). The steps were reviewed in detail with participants whose EKGs were of poor quality. Enrollees were to be contacted for any QTc duration >450 ms or a change of 60 ms from baseline at which time study drug (if applicable) was to be discontinued. Daily temperatures, daily EKGs, regular follow-up questionnaires, and the 14-day saliva SARS-C0V-2 test were still to be done. All tracings were downloaded for subsequent blinded analysis. As a safety measure, if five or more participants demonstrate QTc durations of > 450 ms, the study would be stopped.
Blinded review
After initial EKG review by the cardiologist study investigator for the safety endpoints, the EKGs were subsequently evaluated by a blinded reviewer for the following: quality, rate, PR interval, QRS interval, QTc interval, and any other baseline abnormalities. EKGs were determined of poor quality if they did not demonstrate an isoelectric baseline for three or more consecutive beats or demonstrated ambiguous or low amplitude (<1mV) T-waves. If quality limited evaluation of a measurement, the measurement was not used. Evaluation for upper limb lead reversal was conducted. Rate was determined by average heart rate over a 30-s time interval. All leads were visually inspected to determine the lead with the longest QT interval. Using the selected lead, at least three measurements of the QT interval were made, the longest of which was recorded. The QT segment endpoint was determined by the maximal slope intercept of the T wave. The Framingham formula was used to obtain QTc. All EKGs were evaluated on a computer using the program ImageJ. This allowed pixel measurements be obtained and converted to appropriate time measurements. Each pixel would equate to a time of 4–5 ms depending on the resolution of the image. If there was difficulty, then hand measurements with printed EKGs and calipers were conducted to ensure precision
Study drug
HCQ (Plaquenil®) 200 mg tablets were donated by Advanz Pharma, Bannockburn, IL. Size of the tablet and labeling of the medication as Plaquenil® precluded a double-blinded, placebo-controlled trial. Drug was stored in the Bryn Mawr Hospital Pharmacy, Main Line Health System, and dispensed to enrollees based on a computer-generated randomization table. All members of the same household who chose to participate in the study were randomized to the same group. Twenty HCQ 200 mg tablets for each enrollee in the treatment arm were shipped using United Parcel Service (UPS) overnight delivery.
Clinical monitoring of enrollees and telephone support network
Study participants were instructed to record their temperature twice a day. A follow-up questionnaire documenting symptoms related to COVID-19 infection and potential adverse drug reactions was administered by the study coordinator on days 1, 4, 7, 10, and 14. A 24-h call number to reach a study investigator and or the Office of Research Protections, Main Line Health System was provided. Enrollees were instructed to contact their personal physicians and the study coordinator if any symptoms developed.
Participants’ protected health information was maintained securely on study laptop computers in encrypted files. The goal was a sample size of 170 participants.
3 Results
There were 483 potential household members of COVID-19 patients contacted by telephone or e-mail. No response was received from 209 (43.3%), 90 (18.6%) declined to participate, 32 (6.6%) were not household contacts of the COVID-19 positive cases, and 34 (7%) did not meet inclusion criteria or had already tested positive for SARS-CoV-2. In addition, 40 (8.3%) were excluded because of incompatibilities in telephone, e-mail, language, or comprehension; 4 (0.8%) were outside time window for enrollment; 11 (2.3%) had preexisting health conditions that disqualified them; and 9 (1.9%) were under age 18 years.
Initially 54 (11.2%) of individuals approached consented to participate; 3 withdrew prior to randomization (Fig. 5).
Table 1 summarizes the characteristics of the 51 who were randomized. The average age was 49.6 years for the 31 in the HCQ arm versus 42.9 years for the 19 in the observation arm. Hypertension was the most common underlying medical condition, but one individual in the HCQ arm reported a history of arrhythmia prior to taking the drug, and one in the observation arm had mild mitral regurgitation associated with paroxysmal atrial fibrillation. Concomitant medications were documented for both groups; 12 participants in the HCQ arm and 10 in the observation arm were not receiving any regular medication. Fifty-one participants out of a total of 483 potential were randomized between early June and to the end of September 2020; 32 were assigned to the HCQ treatment arm. Of these 7 withdrew prior to completion, with 25 completing the study. Nineteen were randomized to the observation arm; 2 withdrew prior to completion, leaving 17 who completed. Of the nine participants who withdrew, none experienced adverse events.
Two individuals from the HCQ study arm declined HCQ but agreed to EKG monitoring and follow-up surveys. Their EKGs were analyzed as part of the observation group. The protocol required 15 EKGs in the HCQ and 14 in the observation arms. The mean number of EKGs acquired per enrollee was 9.6. Quality of the tracings was generally good with the majority having measurable PR, QRS, and QTc intervals, and an average of 2.4 EKGs per participant had EKGs of poor quality. Twenty-five of the 42 individuals had at least one EKG without a measurable QTc and six of the 42 participants had EKGs that were incomplete but with a measurable QTc. It was not clear whether deficient EKGs were related to the individual’s technical ability or the quality of the transmission line.
A total of 407 EKGs were obtained from the 42 enrollees completing the study. There was not a single EKG with QTc prolongation meeting the study stopping criteria. In addition, there were no changes in PR interval or QRS duration.
The most frequent lead used for interpretation was lead II 62% (254/407), followed by lead I 27% (111/407), lead III 4% (16/407), and leads avF 3% (13/407) and avR 3% (13/407). Limb lead reversal was noted in 17.1% (69/403) of the EKGs from 21 participants without negatively impacting on the interpretation. One individual had an incomplete right bundle branch block, and one had an intraventricular conduction delay. Both conditions were present on baseline EKGs with no change during the study. Three participants had sinus tachycardia (HR 101–109/min). In two participants, these occurred in a single tracing without recurrence. In the third case, the increased sinus rate was observed in three successive daily tracings. A single individual was diagnosed with transient atrial fibrillation (which had preexisted) and had been randomized to receive HCQ but did not receive the medication. The participant was withdrawn from the study together with her family members at their request, all of whom had negative COVID-19 PCR tests on day 1.
Figure 6 illustrates the mean PR interval on any given day which was between 144–159 ms in the HCQ group and 138–158 ms in the observation group. The mean QRS interval on any given day was between 72–81 ms in the HCQ group and 80–88 ms in the control group. The mean QTc interval on any given day was between 323–383 ms in the HCQ group and 376–390 in the observation group.
Thus, there was no evidence of cardiac toxicity in either group from the 407 EKGs evaluated.
Figure 7 summarizes the clinical symptoms and COVID-19 (SARS-CoV-2 saliva PCR) status pretreatment on day 1 and at study end day 14 of the 42 participants who completed the study. There were two enrollees who were assigned to the HCQ arm but refused drug. They completed other study requirements and were evaluated in the observation group. Seven enrollees had symptoms consistent with COVID-19 during the 2-week study period, while the remainder were asymptomatic. Two participants continued to experience symptoms on D14. Both were assigned to HCQ. Eight individuals had positive SARS-CoV-2 saliva tests at baseline. Two remained positive at day 14. No individuals converted from negative to positive over the 14-day study interval. There were no deaths or hospital admissions.
4 Discussion
This study demonstrates that despite being conceived and operationalized during the peak of the COVID-19 pandemic, it is possible to design and execute a virtual clinical trial incorporating cardiac safety monitoring. Enrollment in the study was significantly impacted by the local intensity of the COVID-19 pandemic and publicity regarding the use of HCQ for coronavirus SARS-CoV-2 treatment and prevention and the optimal dose to use. Ultimately, study events were insufficient to determine HCQ benefit or safety in preventing symptomatic or asymptomatic COVID-19 infections in household contacts of active COVID-19 patients. There were no deaths or serious adverse outcomes. However, remote screening and enrollment of eligible individuals and the use of a newly introduced home diagnostic testing for the virus and home use of smartphone software and hardware for EKG monitoring were successful. After initial training on the mobile EKG application, support and education for ensuring participant compliance with ongoing real-time monitoring and tracing quality was achieved and is recommended for future studies and clinical application. It is also critical to emphasize the importance of investigator availability for technical support. This is also the first time that the use of a remote 6-lead EKG device (KardiaMobile® 6L device) has been reported in a pandemic research setting. Prior published studies of COVID-19 have used portable EKG monitoring devices solely in the inpatient setting [27] or as a one-time validation of the QT intervals as measured by Apple SmartWatches® compared with standard 12-lead EKGs in a variety of treatment settings [28]. There is one case report of a COVID-19 patient monitored at home via an Apple Smartwatch® [29]. The 6-lead device proved to be advantageous over its single-lead counterparts by providing additional leads for EKG analysis: Single-lead devices are only capable of providing information from lead I, but nearly 73% (296/407) of the EKGs in our study were felt to have more reliable and accurate interval measurements in leads other than lead I.
Of interest is the recently published Barcelona Postexposure Prophylaxis Study against SARS-CoV-2 (BCN-PEP-CoV2) [30]. The efficacy and safety of hydroxychloroquine at a single dose of 800 mg followed by 400 mg daily for 6 days were compared to usual care. The goal was to prevent PCR-confirmed and/or symptomatic COVID-19 and SARS-CoV-2 infection in contacts exposed to PCR-positive patients. The efficacy outcome was PCR-confirmed, symptomatic COVID-19 disease. The incidence in the HCQ and usual care group was similar (5.7 vs 6.2%, respectively). No treatment-related serious adverse events were reported in either the HCQ or usual care groups. In comparison, our study included a rigorous EKG component with daily 6-lead EKGs on all analyzed patients, thereby excluding electrophysiologically related abnormalities. The dose of HCQ was lower (200 mg BID) and the duration longer (10 days).
5 Future directions
We believe that larger scale studies with remote monitoring will be possible. Future trials might be conducted during other communicable outbreaks such as seasonal influenza but also more generally in clinical trials. Further study of the 6-lead remote smartphone monitoring application and hardware including optimal timing and frequency of use would increase applicability in other settings.
References
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. https://doi.org/10.1016/S0140-6736(20)30183-5.
Wiersinga WJ, Rhodes A, Chang AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19). JAMA. 2020;324:782–93. https://doi.org/10.1001/jama.2020.12839.
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–7. https://doi.org/10.1056/NEJMc2004973.
Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–82. https://doi.org/10.7326/M20-0504.
Day M. COVID-19: Identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ. 2020;368:m1165. https://doi.org/10.1136/bmj.m1165.
Rolain J-M, Colson P, Raoult D. Recycling of chloroquine and its hydroxyl analogue to face bacterial fungal and viral infections in the 21st century. Int J Antimicrob Agents. 2007;30:297–308. https://doi.org/10.1016/j.ijantimicag.2007.05.015.
Devaux CA, Rolain J-M, Colson P, Raoult D. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int J Antimicrob Agents. 2020;55:105938. https://doi.org/10.1016/j.ijantimicag.2020.105938.
Colson P, Rolain J-M, Lagier J-C, Brouqui P, Raoult D. Chloroquine and hydroxychloroquine as available weapons to fight COVID-19. Int J Antimicrob Agents. 2020;105932. doi.org/10.1016/j.ijantimicag.2020.105932.
Liu J, Cao R, Xu M, Wang X, Zhang H, Hu H, et al. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6:16. https://doi.org/10.1038/s41421-020-0156-0.
Mitja O, Clotet B. Use of antiviral drugs to reduce COVID-19 transmission. Lancet Glob Health 2020;8:e639-e640. doi.org/https://doi.org/10.1016/S2234-109X(20)30114-5
Vincent MJ, Bergeron E, Benjannet S, Erickson BR, Rollin PE, Ksiazek TG, et al. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J. 2005;2:69–78. https://doi.org/10.1186/1742-422X-2-69.
Principi N, Esposito S. Chloroquine or hydroxychloroquine for prophylaxis of COVID-19. Lancet Infect Dis. 2020;20:1118. https://doi.org/10.1016/S1473.3099(20)30296-6.
Marquis-Gravel G, Roe MT, Turakhia MP, Boden W, Temple R, Sharma A, et al. Technology-enabled clinical trials: transforming medical evidence generation. Circulation. 2019;140:426–36. https://doi.org/10.1061/CIRCULATONHA.119.040798.
Turakhia MP, Desai M, Hedlin H, Rajmane A, Talati N, Ferris T, et al. Rationale and design of a large-scale app-based study to identify cardiac arrhythmias using a smartwatch: the Apple Heart Study. Am Heart J. 2019;207:66–75. https://doi.org/10.1016/j.ahj.2018.09.002.
Spaccarotella CAM, Polimeni A, Migliarino S, Principe E, Curcio A, Mongiarado A, et al. Multichannel electrocardiograms obtained by a smartwatch for the diagnosis of ST-segment changes. JAMA Cardiol. 2020;5:1176–80. https://doi.org/10.1001/jamacardio.2020.3994.
Kang Y, Chen T, Mui D, Ferrari V, Jagasia D, Scherrer-Crosbie M, et al. Han Y. Cardiovascular manifestations and treatment considerations in COVID-19. Heart. 2020, 106:1132–41. https://doi.org/10.1136/heartjnl-2020.317056.
Sanofi-Aventis Canada Inc., Product Monograph Plaquenil® (Hydroxychloroquine Sulfate Tablets USP 200mg), August 26, 2019. https://pdf.hres.ca/dpd_pm/00052851.PDF
Hsia B, Greige N, Quiroz J, Khokhar A, Daily J, Biase L, et al. QT prolongation in a diverse, urban population of covid-19 patients treated with hydroxychloroquine, chloroquine, or azithromycin. J Interv Card Electrophysiol. 2020;59:337–45 https://doi.org/10.1007/s10840-020-00822-x.
Gao H, Duan X, Guo X, Huang A, Jiao B. Design and tests of a smartphones-based multi-lead ECG monitoring system. Annu Int Conf IEEE Eng Med Biol Soc. 2013;2013:2267–70. https://doi.org/10.1109/EMBC.2013.6609989.
Perez MV, Mahaffey KW, Hedlin H, Rumsfeld JS, Garcia A, Ferris T, et al. Large-scale assessment of a smartwatch to identify atrial fibrillation. N Engl J Med. 2019;381:1901–17. https://doi.org/10.1056/NEJMoa1901183.
National Institute for Health and Care Excellence. KardiaMobile® for the ambulatory detection of atrial fibrillation. Medtech innovation briefing [MIB232] published 29 2020. Accessed 11-25-20 at https://www.nice.org.uk/advice/mib232/resources/kardiamobile-for-the-ambulatory-detection-of-atrial-fibrillation-pdf-2285965569121477.
Giudicessi JR, Noseworthy PA, Friedman PA, Ackerman MJ. Urgent guidance for navigating and circumventing the QTc-prolonging and torsadogenic potential of possible pharmacotherapies for coronavirus disease 19 (COVID-19). Mayo Clin Proc. 2020;95:1213–21. https://doi.org/10.1016/j.mayocp.2020.03.024.
Cipriani A, Zorzi A, Ceccato D, et al. Arrhythmic profile and 24-hour QT interval variability in COVID-19 patients treated with hydroxychloroquine and azithromycin. Int J Cardiol. 2020;316:280–4. https://doi.org/10.1016/j.ijcard.2020.05.036.
Gasperetti A, Biffi M, Duru F, Schiavone M, Ziacchi M, Mitacchione G, Lavalle C, Saguner A, Lanfranchi A, Casalini G, et al. Arrhythmic safety of hydroxychloroquine in COVID-19 patients from different clinical settings. Europace. 2020;euaa216. doi: 10.1093/europace/euaa216.
Page A, Kocabas O, Soyata T, Aktas M, Couderc J-P. Cloud-based privacy-preserving remote ECG monitoring and surveillance. Ann Noninvasive Electrocardiol. 2015;20:328–37. https://doi.org/10.1111/anec.12204.
U.S. Food and Drug Administration. FDA guidance on conduct of clinical trials of medical products during COVID-19 public health emergency: Guidance for industry, investigators, and institutional review boards. 2020; updated September 21, 2020. https://www.fda.gov/media/136238/download.
González NT, Acosta LA, Miranda DV, Plasencia AI, Caceres VB, Zambrano MR, et al. QT interval measurement with portable device during COVID-19 outbreak. Int J Cardiol Heart Vasc. 2020;30:100644. https://doi.org/10.1016/j.ijcha.2020.100644.
Strik M, Caillol T, Ramirez FD, Abu-Alrub S, Marchand H, Welte N, et al. Validating QT-interval measurement using the Apple Watch ECG to enable remote monitoring during the COVID-19 pandemic. Circulation. 2020;142:416–8. https://doi.org/10.1161/CIRCULATIONAHA.120.048253.
Chinitz JS, Goyal R, Morales DC, Harding M, Selim S, Epstein LM. Use of a smartwatch for assessment of the QT interval in outpatients with coronavirus disease 2019. J Innov Card Rhythm Manag. 2020;11:4219–22. https://doi.org/10.19102/ICRM.2020.1100904.
Mitja O, Corbacho-Monne M, Ubals M, Alemany A, Suner C, Tebe C, et al. A Cluster randomized trial of hydroxychloroquine for prevention of Covid-19. N Engl J Med. 2021;384:417–27. https://doi.org/10.1056/NEJMoa2021801.
Acknowledgements
The authors acknowledge Rachel Bobby (study enrollment), Chris Trent-Davis (administrative support), Advanz Pharmaceuticals (donation of study drug), and AliveCor (assistance with KardiaMobile® 6L software and device).
Availability of data and material
Study database and case report forms are stored by the study’s Principal Investigator (Dr. Kapelusznik)
Code availability
No new coding or new software was developed in this study.
Funding
The study was funded by the Sharpe-Strumia Research Foundation of the Bryn Mawr Hospital, Wistar Morris Cotswold Foundation, Bryn Mawr Hospital, and Mary Lane
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception/design of the work or the acquisition, analysis, or interpretation of data. They have drafted or revised the manuscript, approved the version to be published, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in accordance with the principles of the Declaration of Helsinki. Approval was granted by the Main Line Hospitals IRB (Wynnewood, PA) on May 15, 2020.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Participants signed informed consent forms that stated no identifying information would be revealed in the published manuscript.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, H.H., Ezekowitz, M.D., Columbo, M. et al. Testing the feasibility of operationalizing a prospective, randomized trial with remote cardiac safety EKG monitoring during a pandemic. J Interv Card Electrophysiol 63, 345–356 (2022). https://doi.org/10.1007/s10840-021-00989-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-00989-x