Abstract
Background
Dose escalation of self-injectable biologic therapy for inflammatory bowel diseases may be required to counteract loss of response and/or low drug levels. Payors often require completion of a prior authorization (PA), which is a complex approval pathway before providing coverage. If the initial PA request is denied, clinic staff must complete a time and resource-intensive process to obtain medication approval.
Aims
This study measured time from decision to dose escalate to insurance approval and evaluated impact of approval time on disease activity.
Methods
This was a single-center retrospective analysis of adult patients with IBD prescribed an escalated dose of biologic therapy at an academic center with an integrated specialty pharmacy team from January to December 2018. Outcomes included time to insurance approval and the association between approval time and follow-up C-reactive protein (CRP) and Short Inflammatory Bowel Disease Questionnaire (SIBDQ) scores. Associations were tested using linear regression analyses.
Results
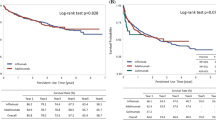
220 patients were included, median age 39, 53% female, and 96% white. Overall median time from decision to dose escalate to insurance approval was 7 days [interquartile range (IQR) 1, 14]. Approval time was delayed when an appeal was required [median of 29 days (IQR 17, 43)]. Patients with a longer time to insurance approval were less likely to have CRP improvement (p = 0.019). Time to insurance approval did not significantly impact follow-up SIBDQ scores.
Conclusion
Patients who had a longer time to insurance approval were less likely to have improvement in CRP, highlighting the negative clinical impact of a complex dose escalation process.



Similar content being viewed by others
References
Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–1517. https://doi.org/10.1053/j.gastro.2004.01.063.
Reinisch W, Sandborn WJ, Hommes DW et al. Adalimumab for induction of clinical remission in moderately to severely active ulcerative colitis: results of a randomised controlled trial. Gut. 2011;60:780–787. https://doi.org/10.1136/gut.2010.221127.
Sandborn WJ, van Assche G, Reinisch W et al. Adalimumab induces and maintains clinical remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2012;142:257–65.e1–3. https://doi.org/10.1053/j.gastro.2011.10.032.
Schreiber S, Khaliq-Kareemi M, Lawrance IC et al. Maintenance therapy with certolizumab pegol for Crohn’s disease. N Engl J Med. 2007;357:239–250. https://doi.org/10.1056/NEJMoa062897.
Sandborn WJ, Feagan BG, Marano C et al. Subcutaneous golimumab maintains clinical response in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2014;146:96–109.e1. https://doi.org/10.1053/j.gastro.2013.06.010.
Feagan BG, Sandborn WJ, Gasink C et al. Ustekinumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2016;375:1946–1960. https://doi.org/10.1056/NEJMoa1602773.
Chao YS, Visintini S. Biologics dose escalation for the treatment of inflammatory bowel disease: a review of clinical effectiveness, cost-effectiveness, and guidelines [Internet]. 2018. https://www.ncbi.nlm.nih.gov/books/NBK537799/.
Little DHW, Tabatabavakili S, Shaffer SR, Nguyen GC, Weizman AV, Targownik LE. Effectiveness of dose de-escalation of biologic therapy in inflammatory bowel disease: a systematic review. Am J Gastroenterol. 2020;115:1768–1774. https://doi.org/10.14309/ajg.0000000000000783.
Baert F, Glorieus E, Reenaers C et al. Adalimumab dose escalation and dose de-escalation success rate and predictors in a large national cohort of Crohn’s patients. J Crohns Colitis. 2013;7:154–160. https://doi.org/10.1016/j.crohns.2012.03.018.
Taxonera C, Rodríguez C, Bertoletti F et al. Clinical outcomes of golimumab as first, second or third anti-TNF agent in patients with moderate-to-severe ulcerative colitis. Inflamm Bowel Dis. 2017;23:1394–1402. https://doi.org/10.1097/mib.0000000000001144.
Greenup AJ, Rosenfeld G, Bressler B. Ustekinumab use in Crohn’s disease: a Canadian tertiary care centre experience. Scand J Gastroenterol. 2017;52:1354–1359. https://doi.org/10.1080/00365521.2017.1373847.
Khorrami S, Ginard D, Marín-Jiménez I et al. Ustekinumab for the treatment of refractory Crohn’s disease: the Spanish experience in a large multicentre open-label cohort. Inflamm Bowel Dis. 2016;22:1662–1669. https://doi.org/10.1097/mib.0000000000000842.
Kopylov U, Afif W, Cohen A et al. Subcutaneous ustekinumab for the treatment of anti-TNF resistant Crohn’s disease—the McGill experience. J Crohns Colitis. 2014;8:1516–1522. https://doi.org/10.1016/j.crohns.2014.06.005.
Ma C, Fedorak RN, Kaplan GG et al. Long-term maintenance of clinical, endoscopic, and radiographic response to ustekinumab in moderate-to-severe Crohn’s disease: real-world experience from a multicenter cohort study. Inflamm Bowel Dis. 2017;23:833–839. https://doi.org/10.1097/mib.0000000000001074.
Qiu Y, Chen BL, Mao R et al. Systematic review with meta-analysis: loss of response and requirement of anti-TNFα dose intensification in Crohn’s disease. J Gastroenterol. 2017;52:535–554. https://doi.org/10.1007/s00535-017-1324-3.
AHIP 2022 Survey on Prior Authorization Practices and Gold Carding Experiences. 2022. Available at https://ahiporg-production.s3.amazonaws.com/documents/2022-Prior-Auth-Survey-Results-FINAL.pdf.
Bhat S, Zahorian T, Robert R, Farraye FA. Advocating for patients with inflammatory bowel disease: how to navigate the prior authorization process. Inflamm Bowel Dis. 2019;25:1621–1628. https://doi.org/10.1093/ibd/izz013.
Carlisle RP, Flint ND, Hopkins ZH, Eliason MJ, Duffin KC, Secrest AM. Administrative burden and costs of prior authorizations in a dermatology department. JAMA Dermatol. 2020;156:1074–1078. https://doi.org/10.1001/jamadermatol.2020.1852.
Kahn SA, Bousvaros A. Denials, dilly-dallying, and despair: navigating the insurance labyrinth to obtain medically necessary medications for pediatric inflammatory bowel disease patients. J Pediatr Gastroenterol Nutr. 2022;75:418–422. https://doi.org/10.1097/MPG.0000000000003564.
Constant BD, de Zoeten E, Stahl MG, Vajravelu RK, Lewis JD, Fennimore B, Gerich ME, Scott FI. Delays related to prior authorization in inflammatory bowel disease. Pediatrics. 2022;149:e2021052501.
Cutler T, She Y, Barca J et al. Impact of pharmacy intervention on prior authorization success and efficiency at a University Medical Center. J Manag Care Spec Pharm. 2016;22:1167–1171. https://doi.org/10.18553/jmcp.2016.22.10.1167.
Livezey S, Shah NB, McCormick R, DeClercq J, Choi L, Zuckerman AD. Specialty pharmacist integration into an outpatient neurology clinic improves pimavanserin access. Ment Health Clin. 2021;11:187–193. https://doi.org/10.9740/mhc.2021.05.187.
Zuckerman AD, Carver A, Cooper K et al. An integrated health-system specialty pharmacy model for coordinating transitions of care: specialty medication challenges and specialty pharmacist opportunities. Pharmacy (Basel). 2019. https://doi.org/10.3390/pharmacy7040163.
Choi DK, Cohen NA, Choden T, Cohen RD, Rubin DT. Delays in therapy associated with current prior authorization process for the treatment of inflammatory bowel disease. Inflamm Bowel Dis. 2023. https://doi.org/10.1093/ibd/izad012.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010.
Harris PA, Taylor R, Minor BL et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. https://doi.org/10.1016/j.jbi.2019.103208.
Lepus CA, Hyams JS. Barriers from third-party payers to biologic use in pediatric inflammatory bowel disease. JPGN Rep. 2022. https://doi.org/10.1097/pg9.0000000000000215.
Agarwal A, Freedman RA, Goicuria F et al. Prior authorization for medications in a breast oncology practice: navigation of a complex process. J Oncol Pract. 2017;13:e273–e282. https://doi.org/10.1200/JOP.2016.017756.
MacKinnon N, Kumar R. Prior authorization programs: a critical review of the literature. J Manag Care Pharm. 2001;7:297–303. https://doi.org/10.18553/jmcp.2001.7.4.297.
Popatia S, Flood KS, Golbari NM et al. Examining the prior authorization process, patient outcomes, and the impact of a pharmacy intervention: a single-center review. J Am Acad Dermatol. 2019;81:1308–1318. https://doi.org/10.1016/j.jaad.2019.05.024.
Howell S, Yin PT, Robinson JC. Quantifying the economic burden of drug utilization management on payers, manufacturers, physicians, and patients. Health Aff (Millwood). 2021;40:1206–1214. https://doi.org/10.1377/hlthaff.2021.00036.
Geynisman DM, Meeker CR, Doyle JL et al. Provider and patient burdens of obtaining oral anticancer medications. Am J Manag Care. 2018;24:e128–e133.
Niccolai JL, Roman DL, Julius JM, Nadour RW. Potential obstacles in the acquisition of oral anticancer medications. J Oncol Pract. 2017;13:e29–e36. https://doi.org/10.1200/jop.2016.012302.
Wang AA, Tapia C, Bhanji Y et al. Barriers to receipt of novel oral oncolytics: a single-institution quality improvement investigation. J Oncol Pharm Pract. 2020;26:279–285. https://doi.org/10.1177/1078155219841424.
Anders B, Shillingburg A, Newton M. Oral antineoplastic agents: assessing the delay in care. Chemother Res Pract. 2015;2015:512016. https://doi.org/10.1155/2015/512016.
Pfeffer J, Witters D, Agrawal S, Harter J. The magnitude and effects of “sludge” in benefits administration: how health insurance hassles burden workers and cost employers. Acad Manag Discov. 2020. https://doi.org/10.5465/amd.2020.0063.
Wyatt H, Peter M, Zuckerman AD et al. Assessing the impact of limited distribution drug networks based on time to accessing oral oncolytic agents at an integrated specialty pharmacy. JHOP. 2020;10:198–205.
Peter ME, Markley B, DeClercq J et al. Inclusion in limited distribution drug network reduces time to dalfampridine access in patients with multiple sclerosis at a health-system specialty pharmacy. J Manag Care Spec Pharm. 2021;27:256–262. https://doi.org/10.18553/jmcp.2021.27.2.256.
Academia EC, Mejías-De Jesús CM, Stevens JS et al. Adherence to oral oncolytics filled through an internal health-system specialty pharmacy compared with external specialty pharmacies. J Manag Care Spec Pharm. 2021;27:1438–1446. https://doi.org/10.18553/jmcp.2021.27.10.1438.
Reynolds VW, Chinn ME, Jolly JA et al. Integrated specialty pharmacy yields high PCSK9 inhibitor access and initiation rates. J Clin Lipidol. 2019;13:254–264. https://doi.org/10.1016/j.jacl.2019.01.003.
Burrus TE, Vogt H, Pettit RS. Impact of a pharmacy technician and pharmacist on time to inhaled tobramycin therapy in a pediatric cystic fibrosis clinic. Pediatr Pulmonol. 2021;56:2861–2867. https://doi.org/10.1002/ppul.25554.
McCabe CC, Barbee MS, Watson ML et al. Comparison of rates of adherence to oral chemotherapy medications filled through an internal health-system specialty pharmacy vs external specialty pharmacies. Am J Health Syst Pharm. 2020;77:1118–1127. https://doi.org/10.1093/ajhp/zxaa135.
Zaepfel M, Cristofaro L, Trawinski A, McCarthy K, Rightmier E, Khadem T. Evaluation of a hepatitis C patient management program at a university specialty pharmacy. Ann Pharmacother. 2017;51:307–314. https://doi.org/10.1177/1060028016683495.
Zobell JT, Moss J, Heuser SM, Asfour F. Impact of pharmacy technicians as part of an integrated health-system pharmacy team on improvement of medication access in the care of cystic fibrosis patients. Pediatr Pulmonol. 2020;55:3351–3357. https://doi.org/10.1002/ppul.25050.
Dunn EE, Vranek K, Hynicka LM, Gripshover J, Potosky D, Mattingly TJ 2nd. Evaluating a collaborative approach to improve prior authorization efficiency in the treatment of hepatitis C virus. Qual Manag Health Care. 2017;26:136–139. https://doi.org/10.1097/qmh.0000000000000137.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Sara Horst has been a consultant for Janssen, Takeda, Abbvie, and BMS. Dr. David Schwartz has been a consultant for Abbvie, Genetech, Gilead, Janssen, Pfizer, Takeda, Tigenix, and UCB. Dr. Schwartz has also received research grant support from UCB and is a data safety and monitoring board member for Tract. Dr. Nisha Shah received research grant support from Pfizer Inc. and AstraZeneca. Dr. Autumn Zuckerman receives research support from Pfizer Inc. and AstraZeneca. Dr. Jessica Fann has been a consultant for Abbvie.
Ethical approval
This research study was conducted retrospectively from data obtained for clinical purposes and approved by the Vanderbilt University Medical Center IRB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An editorial commenting on this article is available at https://doi.org/10.1007/s10620-023-08100-2.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shah, N.B., Zuckerman, A.D., Hosteng, K.R. et al. Insurance Approval Delay of Biologic Therapy Dose Escalation Associated with Disease Activity in Patients with Inflammatory Bowel Disease. Dig Dis Sci 68, 4331–4338 (2023). https://doi.org/10.1007/s10620-023-08098-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-08098-7